It occurred to me that while we may live with our spouses, or close relatives for many years, we don’t always have the same viewpoint as they do on some issues. The same can be said about our friends; we share interests, but also have differences of opinion. Recently, my husband had a health issue. I decided to examine how we each viewed the situation in the hopes that we could appreciate the other’s viewpoint.
My Point: Tony didn’t take his recent health issue very seriously.
Every six months, my husband, Tony, goes to his cardiologist for a checkup and I go with him. But, for a recent visit, I was busy, so I didn’t go. It was just supposed to be a routine follow up visit. He was told 8 years ago that a pacemaker was “in his future.” In the past, every six months he went, everything was normal. Heart issues run in his family, especially among the men, so he is diligent in this aspect of his health, especially since he is in his late ‘70’s. I wasn’t concerned about the visit. He was always deemed healthy and “good to go” from his cardiologist. I was sure this visit was going to be like all of the others.
But this visit was anything but routine. His doctor administered an EKG, and the results concerned him. Tony had to have a pacemaker installed on Monday. He called me from the doctor’s office and told me I had to come and pick him up and take him immediately to the hospital Emergency Room to be admitted. This was Friday, so he would be under observation for the weekend. He was calm when I picked him up, as if he didn’t have a care in the world. Why didn’t I go to that appointment–this is my fault.
Tony’s Counter Point: I research and manage my health issues and with my doctors and medical staff, I am an active part of my health plan.
I disagree with Jan that I didn’t take this situation seriously. I had 8 years to learn about the process and get comfortable with what was going to happen. I think the only surprise I had was the timing. There were no signs leading up to my need to have this done right away. I was feeling fine, just like the 7 years prior to this happening—I had no issues, no warning. Oh, maybe a few incidents of being lightheaded on the golf course, but I chalked it up to the heat. I resolved the issue by just standing straight up at a slower rate. It was just another routine appointment. I don’t know what my doctor saw on the EKG, but I knew it was serious when he told me to call Jan and get to the Emergency Room right away. It was a “meant to be” moment. I also knew that Jan would feel bad that she didn’t come to the appointment with me, but there really didn’t seem to be any reason for her to be there. She tells me all of the time to “drive carefully.” One day I asked her why she says that since she knows I am a good driver. Her answer was that if she didn’t say that to me every time I drove away from her and something happened to me, she would feel that it was her fault for not telling me to be careful.
My Point: Fear of the Unknown.
I started to get really scared once I thought of things that could happen. What if he didn’t survive the surgery? What would “the kids” and I do without him? Stupid things, but everyday things started to loom large in my mind. Tony always opens difficult jar lids for me, and I save him the last hard boiled egg. He does 95% of the dog chores, while I do the laundry. He is the one that “the kids” call when they need help or advice. He’s the only one who knows how to operate the emergency generator. What were we going to do?
Tony was admitted to the hospital with the pacemaker scheduled to be installed on Monday at 8:00 a.m. I found out that during his stay, at one point, his resting heartrate was 26 beats per minute. Critical, at best. Monday couldn’t come soon enough.
Tony’s Counterpoint: For me, there was no “Unknown.”
I know a few people who have had pacemakers installed so I had a good idea of what to expect. I had no fear of not surviving the surgery. I trusted my doctor and his team, and I knew that this procedure was very different from the one my father had many, many years before. I am not the kind of person who “what if’s,” every situation. I wait to see what happens. But I am also a planner. I think my days in Air Traffic Control taught me to not only have a plan, but a back-up plan. I am also not a risk taker. If I felt there was anything that could go wrong with this procedure, I would have sat down with Jan and discussed our options so we could create a plan together.
My Point: I didn’t arrive on time for the surgery, due to the weather and I was frantic.
I was late, but not very. Our son, Tony Jr., came down from Charlotte and took over the driving aspect and in general, making sure I was OK. I don’t know what I would have done without him. Just having him in the house was comforting. I hate driving in the rain and if I had to drive myself, I would have left the car in the middle of the parking lot just to ensure I got to see Tony on time. It was raining, sheets of rain, and traffic was terrible. I literally ran to the Cardiac Care Unit, my heart pounding, fearing he was already in surgery. “Please be in your room,” I prayed. And then I saw him. He was sitting on the side of the bed laughing as one of his nurses took his blood pressure. He seemed to be his usual cheerful self. How could he be so cheerful when I was such a mess?
Tony’s Counter Point: I had no idea about weather or driving conditions, I was just glad to be going in for the surgery and to get this taken care of.
I could tell Jan was upset when she arrived, but I chalked that up to nerves and probably not sleeping well. I was glad Tony Jr., was here to take care of her when I couldn’t. He handles things a lot like I do. He is calm and rational in the face of uncertainty and he was the perfect one to be with Jan. I also can’t say enough about the Cardiac Care Unit at Novant (17th Street location.) They are a caring group of professionals who always had my health and treatment plan top of mind whether we were just casually chatting or they were monitoring my vital signs. They did their best to put everyone at ease. This was routine for them, but they were very aware that each case is different, and they performed each step of the pre-surgery procedures efficiently and effectively.
My Point: It’s over for now….
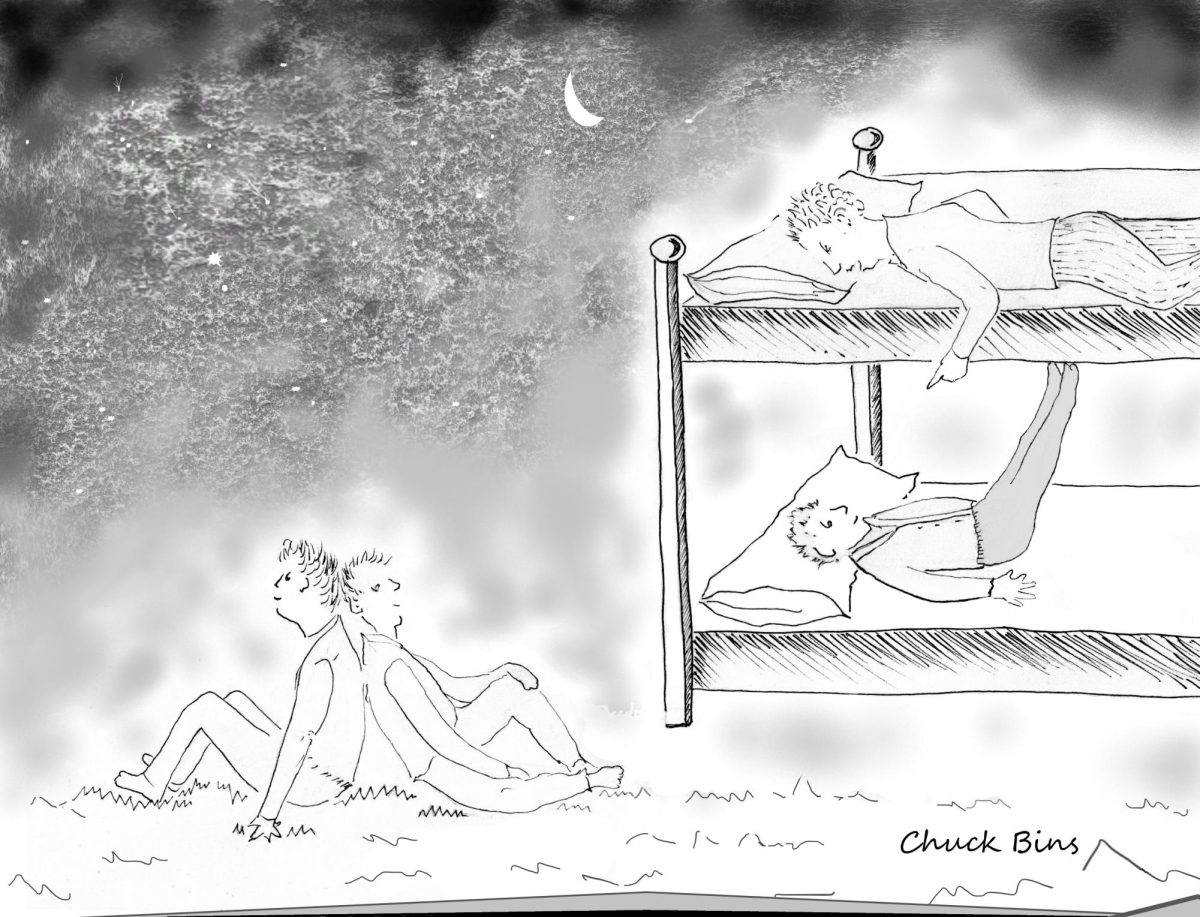
And so, he had the pacemaker put in. All went well. When he was discharged, we brought a monitor home with us. It sits in our bedroom, right across from where he sleeps and sends information to his doctor’s office if there is any shift in Tony’s heart activity. But, what happens next?
Tony thinks that I sleep soundly every night. He doesn’t know that there are many nights when I sit up and just watch that machine. It’s like a lifeline to me. It keeps him safe in a way that I can’t. If I don’t hear Tony sleeping at night, I reach out just to make sure he is OK, and I check to ensure that the heart machine’s green light is still shining brightly. Touching him usually wakes him up; maybe that’s my mission. I just want to know that he is still alive. He is with me, and I am happy. I know that “for now,” is the best we can have.
Tony’s Counter Point: I am at peace with my mortality…
That doesn’t mean I have a death wish, but I am pragmatic about my longevity. I am in my late ‘70’s and I have lived what I consider to be a good life. I hope I get more time on this earth with Jan, our children, our grandchildren, family and friends, but I have very few regrets about how my life turned out. I tend to look on the bright side of things. Some people who have had pacemaker installed actually name them. A friend of mine named hers “Thumper.” I thought it was funny at first, but after thinking about it, I thought, “why not? It is a part of me now and it keeps me going. I named mine, “Sparky.” Not only is it a conversation started, I think it reflects my personality!
Jan and I don’t see eye-to-eye on many things. But we make our life work every day with patience for each other and compassion.
My point is, that’s what marriage is all about.
My Point: Yes, dear!